NHS Test and Trace performance tracker
13 May 2021
About this tracker
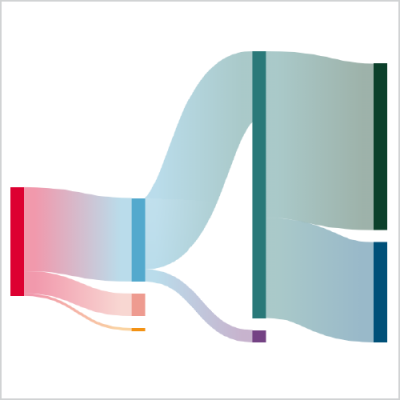
- The NHS Test and Trace (NHSTT) system aims to control the spread of COVID-19 in England by ensuring that people can be tested when necessary, and by identifying close contacts of people who have tested positive (positive cases) and asking them to self-isolate.
- The government’s Scientific Advisory Group for Emergencies (SAGE) has recommended that at least 80% of close contacts of positive cases must be reached for the system to be effective.
- In this tracker, we monitor and reflect on the performance of NHSTT, analysing the latest statistics on the number of positive cases reached and the number of contacts who were asked to isolate each week from the launch of NHSTT on 28 May 2020 to 5 May 2021.
- The tracker's final regular update was on 13 May 2021 with additional data covering 29 April to 5 May 2021.
Key points: 29 April to 5 May 2021
- Nearly a year after NHSTT was launched, this will be our last regular update to the performance tracker. As case numbers have dropped and contact tracing performance has stabilised, the current policy debate has instead shifted towards the timing and extent of the government’s recovery roadmap, and how this might be impacted by variants of concern.
- Testing and contact tracing of course remains critical through this, but is now a less volatile space than at other points over the past 12 months. Furthermore, the ongoing changes to policy on testing – including testing for people without symptoms, the use of PCR tests, and the role of testing for people who are fully vaccinated – makes it ever more challenging to interpret trends in test use and case numbers.
- However, it remains clear that testing remains just one part of the pandemic response that should never be thought of in isolation. The impact of testing on transmission is intricately related to contact tracing performance and isolation support, to the vaccine roll-out, and to the wider social and economic circumstances in which people find themselves.
- Time and again research has shown how more vulnerable and deprived population groups – people in crowded housing and on low incomes, with caring responsibilities or in insecure employment, people from minority ethnic groups – have been disproportionately impacted by the pandemic, are less likely to access regular testing, are less likely to be able to adhere to isolation guidance, and have consistently worse outcomes.
- These disparities will simply continue to widen inequalities unless COVID policy – both with test and trace as well as the broader government COVID policy on housing, employment and welfare – is targeted at, and co-designed with, the very people who need it most. Nobody should be worse off for having to isolate.
- This week, we see that case numbers continue to fall with just 14,313 reported (down 9% on the previous week), as do the numbers of people being tested (down 7% to 4.61m). This is largely due to changes in the use of rapid LFD tests for people without symptoms – nearly two thirds of the reduction being down to fewer tests done in secondary schools and colleges.
- And when it comes to differences in LFD testing rates, there is a significant range across the country – from a low of 3,400 tests per 100,000 in the London Borough of Tower Hamlets, to a high of 15,100 tests per 100,000 in Rutland and 13,900 per 100,000 both in Wokingham and in North Somerset. We’ll be expanding on some of these differences and how they may relate to case rates and inequalities in a separate piece of work in the future.
- When it comes to contact tracing, performance is largely unchanged: 91% of cases were reached with 82% providing details of close contacts. However, the percentage of contacts reached has dropped over the past 6 weeks, from 90% to 84%. This has been mainly due to fewer contacts being from the same household as the case – falling from 66% to 46% of contacts over the same period – and that these contacts are inherently more difficult to reach.
- Furthermore, the proportion of overall cases among international travellers will have impacted on contact tracing. In the 2 weeks from 22 April to 5 May 2021, over 800 international arrivals tested positive, and the preceding 2 weeks it was over 1,400 arrivals. In these circumstances, contact tracing everyone on an aircraft is inherently more arduous and time consuming. This is reflected in test and trace end-to-end time where the percentage of contacts reached within 3 days of the case being tested fell from 80% at the end of March to 59% two weeks later, before picking up to 68% in the most recent week.
- Finally, rising case rates seen in places such as Bolton and Blackburn with Darwen (places that have borne the brunt of pandemic throughout the past 15 months) raises concerns that the spread of new variants of concern may yet again devastate those same largely socioeconomically deprived communities. This highlights how future policies have to address the underlying drivers of inequalities, such as insecure work and poor housing, that fuel viral spread if we are to tackle the virus and realise a genuinely inclusive socioeconomic recovery.
Key points from previous weeks
- After a dip over the Easter bank holiday weekend, the number of people being tested increased by 15% to 4.4m in the week ending 14 April, but this is still some way off the peak of 6.2m four weeks earlier.
- The changes have been mainly due to variation in the use of rapid lateral flow devices (LFDs). These have been rolled out by the government in a range of settings over recent months and are now available to everyone in England. They are designed to be used by people without symptoms, providing a result within 30 minutes.
- The drop in LFD use in the last week of March and first week of April (down from 7.1m tests a week to just 4.0m) was a result of fewer tests being done by staff and pupils from secondary schools and colleges. The fall coincided with the shift to testing at home for students and pupils, and the start of the Easter holidays.
- In the most recent week, however, LFD use was up by 750k. Only a fifth of this rise is explained by school testing, with the rest coming other government testing schemes – in particular LFDs being made available to everyone from 9 April 2021.
- There are still important differences by region. The highest LFD use is in the East of England with 12,500 tests per 100,000, compared to just 5,200 per 100,000 in London. This will partly be explained by the different dates that schools returned across the country, but also due to differences in factors such as employment, access, and willingness to engage with the scheme. In the coming weeks it will be important to monitor how testing uptake varies now that everyone is entitled to use them.
- Despite the 15% increase in the number of people being tested, case numbers still fell by 9%. Whilst overall NHSTT performance remains broadly unchanged, there is an increasing trend in the time taken to reach contacts from when a case is first passed to the system.
- The number of contacts per case is still rising, with 4.2 contacts per case identified in the most recent week and just half being from the same household as the case. By comparison, over 80% of contacts were from the same household eight weeks before.
- As more contacts are identified per case, and more of these are from outside of the case’s household, the median time for contacts to be reached from when a case first developed symptoms is now 97 hours, up from just 79 hours two weeks previously.
- As society continues to open up, any additional time gives more opportunity for the virus to spread, so it’s important that this trend doesn’t continue. And as ever, these numbers don’t tell us about who doesn’t get tested and who struggles to adhere to isolation. As the number of cases in the community falls and social mixing increases, it becomes ever more important that any cases that do occur are identified and managed as quickly as possible before the virus has the chance to spread.
- For two weeks in a row, the number of people getting tested each week has dropped. This is despite the ever-increasing availability of rapid lateral flow devices (LFDs) for people without symptoms.
- In the most recent week (ending 31 March), the number of people tested overall fell by 18% from 5.9m to 4.8m. This was due to a drop in the number of LFD tests, particularly among secondary school students, rather than changes to the number of people using PCR tests which remained largely unchanged.
- There were 5.5m LFD tests used in the most recent week, 23% fewer than 7.1m the week before. Among secondary schools and colleges the drop was 33%, from 4.6m to 3.0m. This will partly be due to schools closing for holidays in the week commencing 29 March, but it also coincides with secondary school testing moving to being done at home rather than on school premises which may have led to reduced test uptake.
- There were also differences in LFD use by region and upper tier local authority. The South West region had the highest rate of LFD use with 12,224 LFDs per 100,000 population in the most recent week, nearly double the rate in London at just 6,877 LFDs used per 100,000. The differences by local authority were even larger, ranging from 3,045 LFDs used per 100,000 in Tower Hamlets, to 16,026 per 100,000 in North Somerset.
- These differences will be due partly to variations in the proportion of people eligible for the various government testing schemes, but may also represent differences in knowledge of test availability, willingness to get tested, or test access and availability.
- The number of contacts identified per case also continued to increase, and it has done for the past six weeks in a row.
- On average, there were 3.6 contacts identified per case, up from 3.4 the week before, and significantly higher than the low of 2.0 in the middle of February. Whilst the percentage of cases providing details of close contacts has remained largely unchanged over the previous two weeks – as has the percentage of contacts that are from the same household as the case – this does suggest more social mixing as lockdown measures were lifted.
There were two stories this week – lots more testing and increasing numbers of contacts per case.
Testing
- As schools returned there were a remarkable 5.8m people tested from 4 to 10 March 2021. This is more than 10% of the entire population of England tested in a single week, and an 85% increase on the preceding week.
- Of the 5.8m people tested, 5.4m were community tests – or pillar 2 tests. This is the kind of population level testing that was unimaginable back when schools re-opened in September last year and testing struggle to match demand with pillar 2 capacity at around 1m tests per week across the whole of the UK.
- The increase is due to the growing use of lateral flow devices (LFDs), particularly in secondary schools. LFDs are rapid tests that aim to identify cases without symptoms and there were 6.3m of these tests taken in the week ending 10 March 2021, compared with 2.8m the previous week (many people will have taken more than one LFD test). And of these 6.3m tests, 3.7m were taken by secondary school children and staff – 3m more than the previous week. NHSTT now publish a separate LFD testing report.
- There is also some substantial variation in LFD use across the country. The region with the lowest LFD use per head is London at 8,937 per 100,000 compared with 12,505 in the East of England.
- Finally, it’s worth noting that the LFD tests reported are only those registered through the National Testing Programme digital infrastructure. This doesn’t include a large proportion of secondary care NHS staff testing at home, as well as some test done in the private sector testing meaning the actual number of people being tested with LFDs in the last week will even larger.
Contacts per case
- Of the 36.5k cases handled by NHSTT, 32.4k were reached (89%) – similar to previous weeks – but 82% gave details of close contacts and 2.7 contacts were identified per case. Both measures were previously at that level in October last year.
- This is reflected in over a quarter of contacts not being from the same household as the case, again something not seen since before the November lockdown and an increasing sign of more social mixing now that schools have returned. One thing that it isn’t possible to tell from the data, however, is whether the increase number of non-household contacts is driven entirely by returning school pupils, or if there’s also a wider behavioural change taking place as society begins to reopen.
- In the week commencing 18 February, 2.8m people in England were tested for COVID-19. This is less than the 3.0m people tested two weeks before, but a 9% increase on 2.6m people tested from 11–17 February.
- The rise in the number of people being tested is entirely due to testing in the community (pillar 2, rather than testing among those who are clinically unwell or health and care workers which comes under pillar 1). More specifically, the increase is due to greater use of lateral flow devices (LFDs). LFDs are rapid tests used to identify cases among people without symptoms. They are increasingly being rolled out in schools, workplaces, and more generally among people who are unable to work from home.
- The number of LFD tests done increased by 470k compared with the previous week to 2.2m (note – people will often take more than one LFD in a given week). By contrast, the amount of pillar 2 PCR tests done fell by 17K and remains at around 1.1m.
- Increased use of LFDs to find cases that are otherwise asymptomatic is a key part of the government’s roadmap to easing restrictions, and currently there is a particular focus on education settings before schools return next week. In the most recent week reported, education settings accounted for 45% of LFD tests used and of the 470k additional LFDs used compared with the previous week, 410k were in educational settings as pupils returned from half term. However, overall LFD use is still lower in the most recent week compared to two weeks previously. We will be tracking LFD use by region and setting more over the coming weeks.
- On contact tracing, the number of cases identified in the week commencing 18 February fell by 19% to 69k, and the proportion of cases and contacts reached by NHSTT remained similar to previous weeks at 88% and 93% respectively. The time taken for results to be reported and for contacts to be told to self-isolate increased very slightly. It took a median of 79 hours between a case getting symptoms to their contacts being reached compared with 77 hours in the previous week.
- It’s also worth noting that the percentage of close contacts identified who are from the same household as the case has fallen two weeks in a row from 87% to 84%. While this percentage is still high, it may be a sign that people are increasingly leaving home and mixing outside of household groups.
- Finally, these data tell us nothing about who isn’t getting tested and how readily people are able to adhere to isolation guidance. The roadmap sets out some welcome proposals to help support people needing to isolate, but more will be needed to overcome many of the structural barriers to isolation such as insecure employment, overcrowded housing, and deprivation.
- Despite case numbers falling by between 25% and 30% over each of the past three weeks, the number of people being tested has remained high at 3m per week.
- This has been due to increased use of lateral flow devices (LFDs) – rapid tests providing results within 30 minutes and generally used to identify cases without symptoms that might otherwise transmit disease. The settings using LFDs include schools, care homes, and some workplaces, as well as community testing sites set up by local authorities, often for people who are unable to work from home.
- The number of LFD tests taken has increased by 35% over the last two weeks to 2.4m, a five-fold increase in use since the start of January. By contrast, the number of PCR tests taken has fallen by 13% from two weeks ago to 1.3m.
- It will be important to track how the use of LFDs varies among different populations, particularly those who are more socioeconomically deprived. Testing policy should ensure that variation in LFD availability and acceptability doesn’t place people who are most vulnerable from harms such as job loss.
- Overall testing turnaround times and contact tracing performance remains similar to previous weeks. For PCR tests done in-person, 85% of results were received within 24hrs and for home testing and satellite test centres (generally care homes), 81% of results were received within 48 hours.
- Of the 106,000 cases handled by NHSTT, 92,000 (87%) were reached and 191,000 contacts were identified – around 2 contacts per case of which 94% were reached.
- NHSTT has now started publishing end-to-end timings, meaning the average (median) time taken to reach a contact from when the case first reported developing symptoms. In the most recent week this was 78 hours, the lowest so far and nearly half of the 143 hours recorded at the start of October.
- So whilst the speed and reach of NHSTT is consistently staying relatively high, it’s important to note that these data don’t tell us about people who don’t get tested despite having symptoms, and people who don’t fully comply with isolation guidance. Work is still needed to ensure that everyone can be confident they will have the social, practical, and financial support required if they do test positive, and that their job – however insecure – will not be put at risk.
- The number of people testing positive for COVID-19 has now fallen for three weeks in a row, but the 196,000 positive cases reported in the most recent week is still 28,000 more than the case numbers at the peak of the second wave in early November.
- Despite falling case numbers, the number of people being tested is the same as two weeks previously – 2.9m people, or 5% of the population. But this is due to the increasing use lateral flow devices among people without symptoms – rapid tests that provide results after just 30 minutes. The number of lateral flow tests taken was 1.8m in the week ending 27 January, up 80% from 1.0m two weeks previously. (Note: that’s not the same as 1.8m people being tested as these kits are often used on multiple occasions by the same person.) Over the same time period, the number of PCR tests taken by people in the community who do have symptoms (pillar 2 testing) fell from 2.1m to 1.5m.
- Looking at test performance, the speed at which people are getting their PCR test results is as good as it’s ever been. Over four out of five people being tested in person in the community (ie those visiting a test site) received their results within 24 hours, and over 97% received their results the day after the test was taken.
- And of the 199,000 cases handled by Test and Trace and the 359,000 contacts identified, 86% of cases and 94% of contacts were reached and advised to isolate. These are both in line with performance seen over recent weeks.
- However, there remain significant differences in the percentage of cases and contacts reached by local authority. Since Test and Trace launched on 28 May 2020, 78% of cases have been reached in Birmingham compared to 94% in Havering. For contacts, the gap is even wider, with 62% reached in Bradford compared with 89% in Thurrock.
- The impact of Test and Trace on slowing viral spread is reliant on people getting tested when they have symptoms, and then people isolating when necessary. UCL’s COVID Social Study recently reported that among the 70,000 people surveyed, only a third of people requested a test every time they developed symptoms, and a third didn’t isolate for at least 10 days despite being symptomatic. Whilst Test and Trace internal performance remains as strong as ever, it needs to be complemented by comprehensive isolation support measures that act to narrow rather than exacerbate existing health and economic inequalities.
- In a sign that the number of infections in the third wave may have now peaked, the number of positive cases reported in the week ending 13 January fell for the first time since the start of December, down 15% to 331,000. However, this is not the case for those aged over 80 years, where the number of people testing positive was up 8% to 20,568. This is the population group most vulnerable to severe infection.
- An astonishing 5% of England’s population – 2.9m people – were tested in the most recent week, up from 2.6m the week before. This increase has been partly due to more people being tested in NHS and PHE laboratories (pillar 1 tests, up 20% to 521,000) and also due to an increase in the use of rapid lateral flow devices for people without symptoms. The number of these tests used has doubled in just a week from 485,000 to 972,000 (note, because multiple lateral flow devices are often used by the same person, this doesn’t mean 972,000 people were testing using these devices).
- Looking at contact tracing, 87% of cases passed to the system were reached by Test and Trace, as were 93% of contacts (similar proportions to previous weeks), but the percentage of cases reporting close contacts has been falling since the start of lockdown, to 75% of cases from 80% two weeks ago.
- Furthermore, the average number of contacts reported per case has been slowly falling in recent weeks, down from 2.5 contacts per case at the start of December to 2.0 reported this week. This includes both the week of Christmas and the following week both having fewer contacts per case than the week ending 23 December, despite easing of social restrictions over Christmas itself.
- Whilst some of this decline may be explained by increased social restrictions, it remains likely that some cases are not reporting all of their contacts. There are many reasons for this, including people unwilling to place others who they live or work with under a legal duty to isolate, particularly in circumstances where that means the contact may be unable to work or fulfil caring responsibilities. Such circumstances are known to be barriers to complying with self-isolation guidance, and can be overcome with increasing the availability of financial and practical support.
- There have been marked changes to NHS Test and Trace performance since the previous update on 3 December 2020.
- The number of people testing positive is rising steeply, almost tripling in three weeks to 311,000 positive cases between 24–30 December. This is alongside a 30% drop in the number of people being tested this week compared to last, to 1.85m people.
- As test demand increased in the first three weeks of December, the time taken to get results for PCR tests in the community started to increase markedly. For example, the median length of time for people to get a result from a regional test site rose from 21 hours to 38 hours. In the most recent week reported, the time taken for results has improved across all test routes alongside the fall in test demand, but is still not back to where it was three weeks before, which for regional test sites was 29 hours. It is crucial that people can get results quickly to reduce the amount of time between symptom onset and the start of contact tracing.
- Contact tracing performance has remained fairly consistent over the month of December despite rising numbers of cases being handled. In the week starting 24 December, 270,000 people were transferred to the system, 229,000 (85%) were reached and 494,000 contacts were identified. This is nearly 300,000 more contacts than just three weeks before.
- An impressive 92% of contacts were reached and asked to isolate, a consistent figure seen throughout December since NHS Test and Trace changed how they manage multiple contacts in the same household (since 27 November, a case can take responsibility for informing household contacts about their need to isolate rather than contact tracers phoning each contact individually).
- Finally, after week-on-week improvements, the percentage of cases reached within 24 hours has dropped to 73% from 80% in the previous week. This has implications not only for the speed of identifying contacts, but also for local authority-led contact tracing systems that take on cases that the national team are unable to reach within 24 hours. The dip in performance may be because of having to adapt processes over the Christmas holiday period, and it will be important to monitor how performance here changes in the coming weeks.
- The number of people testing positive has fallen by a third from two weeks ago, with 111,000 positive cases between 19–25 Nov.
- The number of people getting tested has also reduced over this time period, which has coincided with improvements in the time taken to receive results. For example, now 72% of people using home test kits get a result within 48 hours compared to 57% the week before.
- As the number of people testing positive has fallen, so have the number of cases being transferred to NHSTT. There were 116,000 cases transferred of which 99,000 were reached (85%), and 247,000 contacts identified.
- While percentage of cases reached by NHSTT has stayed the same, the percentage of contacts reached has jumped to 73% from 61% the week before. This is because NHSTT has changed how they manage household contacts under 18. Instead of having to separately reach all contacts who are under 18 years, the parent or guardian can take responsibility. This makes sense and ensures that households receive fewer calls. Plus, the immediate impact of this change on performance suggests the change has been welcomed by households. The improvement in percentage of close contacts reached is entirely due to improvements in reaching household contacts. For non-household close contacts, the percentage reached remains at 64%.
- And of course, being able to record reaching these household contacts at the same time as phoning the case has done wonders for the overall timeliness of contact tracing. The percentage of contacts reached within 24 hours of a case being identified has increased to 61% from 44% the week previously.
- The system still needs to improve however. Underlying all this remains the fact that over 17,000 cases weren’t reached by NHSTT, and only around 60% of the contacts of identified cases are being reached (based on 85% of cases reached, and 73% of their identified contacts), still far from the 80% level recommended by SAGE.
- After two weeks of improvements, NHS Test and Trace performance has stalled whilst the number of people testing positive continues to rise.
- Nearly 157,000 cases were transferred to the system in the most recent week, up from 142,000 the week before. However, the number of contacts identified remained largely the same at around 314,000. This is because the number of contacts per case has fallen over the past few weeks, possibly a result of increased social restrictions.
- The percentage of contacts reached by NHS Test and Trace remains just 61%, a figure that’s barely changed for the past five weeks. This means that optimistically, 51% of the contacts of known cases are being reached (based on 84.9% of cases reached and 60.5% of contacts), far lower than what is needed to meaningfully limit disease spread.
- Finally, the data provided still don’t show the contribution of local contact tracing systems to overall NHS Test and Trace performance, and the updated local authority data highlight huge variation in the proportion of cases and contacts reached in different parts the country – the percentage of cases reached ranges between 71% and 93%, and for contacts it ranges between 49% and 68%.
- Local contact tracing systems are being implemented across the country to work with NHS Test and Trace and reach cases the national team are unable to contact. As we move into winter, they are likely to play an important role in improving overall NHS Test and Trace performance, alongside ensuring that people who are identified as cases and contacts have adequate financial and practical support whilst isolating.
- Between 22–28 October, nearly 140,000 cases were handled by NHS Test and Trace, 16% more than the previous week and a nine-fold increase since the start of September. Despite this rapid increase, the system has consistently been able to reach over 80% of cases, however the percentage of contacts reached stubbornly remains at 60%.
- This means that whilst 115,000 cases and 196,000 contacts were reached and advised to isolate, over 24,000 cases and 131,000 contacts weren’t. And the system is still far from achieving the 80% of contacts needed for the effective system recommended by the government’s Scientific Advisory Group for Emergencies (SAGE).
- Encouragingly, the time between taking a test and getting results is falling and the percentage of cases being contacted within 24 hours has increased to 67%. This is a significant improvement on just 44% the week before. The widespread use of rapid test kits may help to further improve the time it takes to receive test results, but this is still being piloted and not yet available across the country.
- The number of people testing positive keeps rising, up 12% from last week to over 100,000 this week for the first time. And of the 96,521 that were passed to NHSTT, call handlers were still able to reach 81% of cases.
- But things are taking longer. The median length of time taken for people to receive test results for in-person tests (regional, local and mobile test sites) has jumped from 28 hours last week to 45 hours this week. The proportion of non-complex cases reached within 24 hours of being passed to NHSTT has fallen to 54% compared with 77% at the beginning of September (with implications for local contact tracing teams – see last week’s entry below). And the proportion of their contacts reached within 24 hours of the case being transferred to NHSTT is now just 32% compared with 52% back in early September.
- And while the proportion of cases being reached remains high, the proportion of contacts reached has fallen for the fourth week in a row to 60% of all contacts. But rather than this being due to worsening call handler performance, it’s mainly a result of non-complex contacts (where there is a lower success rate of being reached compared with complex contacts) making up a higher proportion of all contacts this week compared to the week before.
- The average number of contacts per case for the 76,096 non-complex cases transferred to NHSTT is the same as last week, but for the 1,796 complex cases, the average number of contacts has fallen from 29 per case three weeks ago to just seven per case this week. This may just be due to chance, but it also may represent a combination of better social distancing, more limited social mixing, and appropriate use of personal protective equipment (PPE) in care settings.
- On 2 October, the national system identified an error in how pillar 2 cases are transferred to contact tracing. This meant that 15,841 cases (from 25 September to 2 October) that hadn’t previously been sent through to NHS Test and Trace (NHSTT) were transferred in bulk on 3 October. Therefore, this week’s data include 11,000 cases transferred to NHSTT that would have ordinarily been dealt with the previous week.
- This week the percentage of cases reached increased from 75% to 77%, and the percentage of cases providing details of contacts also rose from 83% to 85%, its highest since NHSTT began. This shows a slight improvement but doesn’t tell the whole story.
- There were still 20,000 cases that weren’t contacted by NHSTT, and of those cases providing details of contacts, the average number of contacts per case has dropped significantly. This could be due to several factors including people not mixing as much due to increased social restrictions. Correspondingly, the percentage of all contacts that are from the same household as the case has been rising for four weeks in a row, from 57% in the first week of September to 66% in the most recent week.
- Local contact tracing systems are being set up across the country - around half of local authorities now have one in place. Generally, these local systems follow up local cases that the national team hasn’t reached within the first 24 hours of being transferred to NHSTT. Their workload in recent weeks has not only been affected by rising case numbers, but also by significant delays in how long the national team takes to reach cases. The percentage of cases reached within 24 hours has fallen for four successive weeks, and now stands at just 56% of all cases transferred, down from 77% in the first week of September.
- The percentage of contacts of non-complex cases that NHSTT reaches is also falling, and is now just 58% compared with 64% two weeks ago. This may partly be down to difficulties in reaching contacts from cases whose transfer to NHSTT was delayed, but when factoring in evidence that as little as 11% of contacts may actually comply with isolation rules, the implications for containing transmission are significant. These issues are exacerbated by how long it’s now taking for NHSTT to reach contacts and advise them to self-isolate. The proportion of close contacts reached within 24 hours of either the contact or the case first being identified is now at an all-time low of 61% and 39% respectively.
Useful definitions
- Cases are people who have had a positive antigen swab test.
- Cases managed by Public Health England local health protection teams (HPTs) are those linked to outbreaks, for example someone who works at or recently visited a hospital or care home. These cases were previously known as complex cases. All other cases are not managed by local HPTs and were previously known as non-complex cases.
- Close contacts are defined as anyone who a case has had face-to-face contact with (within 1 metre), spent more than 15 minutes within 2 metres of, travelled with in a car, or sat close to on a plane.
-
Polymerase Chain Reaction (PCR) tests are laboratory-based tests which test for the presence of COVID-19 using a swab, which is processed in a laboratory via PCR. They are carried out within pillar 1, pillar 2 and pillar 4.
-
Lateral Flow Device (LFD) tests are swab tests that do not need to be processed in a laboratory and give results in less than one hour. LFDs were first available from 21 October 2020 in limited capacity and in some areas with mass testing pilots. Mass testing is now available nationwide including in workplaces where the same person may take multiple tests. Prior to 27 January 2021, people with positive LFD tests were required to take a confirmatory PCR test before being transferred to the Test and Trace system. From 27 January 2021, positive LFD tests are transferred to the Test and Trace system without the need for a confirmatory PCR results, with the exception of NHS England staff, adult social care, primary school teachers and hauliers.
Further reading
Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
View current vacanciesThe Q community
Q is an initiative connecting people with improvement expertise across the UK.
Find out more

