How is COVID-19 changing the use of emergency care?
15 May 2020
Key points
- The NHS provides universal health care for patients across a wide range of interlinked services and settings. To provide the most complete picture of how COVID-19 has affected people’s access to care, it is important to consider changes in activity across multiple different services.
- On 14 May it was announced that A&E visits were 57% lower last month than in April 2019. This blog discusses the potential drivers of this fall and considers the drop in A&E visits by A&E type, alongside emergency admissions via A&E and ambulance incidents. The aim is to provide a broader perspective on the changes that have happened within the emergency care sector.
- A&E visits across all unit types dropped by 57% in April, but the percentage fall was larger in minor A&E units (71%) than in major A&E units (48%). This is consistent with people with less severe conditions being directed to other NHS services or choosing to avoid seeking medical care. Public Health England surveillance reports also suggest that some of the falls are the result of reductions in the prevalence of certain infectious diseases during the lockdown.
- Emergency admissions through A&E have fallen by less than A&E visits, dropping 37% in April 2020 relative to the same month the year before. This is likely to reflect both a change in the types of patients arriving at A&E, and efforts to reduce the risk of non-COVID patients being infected and to protect capacity.
- There were relatively small changes in ambulance incidents, with a rise of 5% in March and a fall of 4% in April, relative to the same months the year before. However, there have been substantial changes in how ambulance crew treat patients. The number of patients transported to A&E by ambulance in April 2020 was 29% lower than in April 2019. This is a reduction of 4,000 patients per day or 120,000 across the whole month, equivalent to 19% of the overall drop in A&E visits at major units in April 2020 relative to April 2019. There has been a corresponding increase in the number of people who are treated at the scene.
- There are several factors driving the fall in A&E visits in March and April. The reduction in visits for acute conditions such as stroke and heart attack remain a concern. However, it is important to also consider potential reductions in the prevalence of some health conditions and the ways in which NHS services have adapted to keep people out of hospital where possible.
Introduction
The NHS provides universal health care for patients across a wide range of services and settings, but the coronavirus (COVID-19) pandemic has already led to rapid changes in how people are using those services. To understand how the COVID-19 crisis is affecting people’s access to care, analysis must avoid too narrow a focus on individual points on a pathway or settings of care. In some cases, this would miss some of the important changes that have taken place, and could lead to misleading conclusions. But there is much to be learned from looking across multiple services to understand these rapid changes to NHS activity and to begin to assess their potential impact on the quality of care, cost of services and outcomes for patients.
Three drivers of changes in NHS activity
The unprecedented and swift changes in NHS activity since mid-March have been widely reported. Hospitals have experienced a large inflow of COVID-19 patients – rising from virtually no admissions in early March to a peak of just under 21,000 patients in UK hospitals with COVID-19 by mid-April. This large surge in patients has been managed, in part, by reducing planned care, but we have also seen a fall in emergency admissions for non-COVID patients. Some of this will reflect lower demand as the lockdown measures change patterns of need, but in other areas, such as cancer and cardiovascular disease, there are concerns that the reduction in care received may lead to poor outcomes for patients.
There are three main drivers that could be behind these changes:
- Policy choices made in order to create capacity for COVID-19 patients or to protect non-COVID patients and staff: Examples include cancelling planned operations and the movement of most primary care appointments to the telephone or online.
- Changes in patient behaviour, who may choose to use a different NHS service, delay or not seek health care at all: The implications of these changes for patient health will vary by condition. There has been particular concern about the implications of a delayed cancer diagnoses and an initial reduction in A&E visits for acute conditions such as stroke and heart attack.
- Changes in the prevalence of some conditions: While the prevalence of COVID-19 increased rapidly through March and the first half of April, the lockdown has reduced the prevalence of other infectious diseases. This is evidenced by the greater than average fall in hours of GP appointments related to infectious diseases, particularly among children, and greater than average reductions in A&E visits related to gastroenteritis. We might also expect reductions in admissions related to pollution. A University of York study highlighted that nitrogen dioxide levels fell by more than a third in many major cities during March.
The relative importance of these drivers will vary across services, health conditions, and patient characteristics. Trying to understand the full implications of these changes to patient health and subsequent health care needs will be a task for many months and years to come.
What has happened to emergency care use?
One change that has caused great concern is the rapid drop off in A&E use after the lockdown began. On 14 May it was announced that A&E visits were 57% lower last month than in April 2019.
This blog takes a broader look at how activity in the emergency care sector has changed since the start of the pandemic, by examining patterns of A&E visits alongside emergency admissions to hospital through A&E and ambulance incidents.
In a future blog we will examine how these patterns vary across regions. This will be followed by an analysis of differences by type of condition in A&E and emergency admissions, which will help identify areas of harm and shed new light on what is driving the changes in activity.
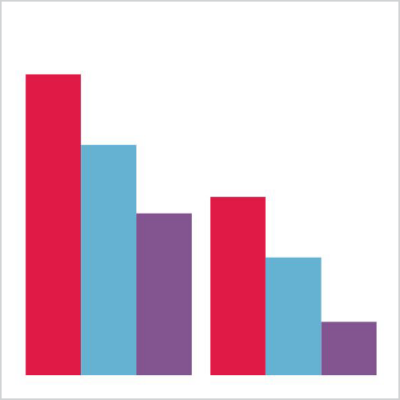
The first figure below shows the average number of daily A&E visits by A&E type, emergency admissions through A&E by A&E type, and ambulance use in February, March and April 2020. The second figure presents the same information but displayed as percentage changes in activity compared to the same months in 2019.
A&E visits
Starting with A&E visits, the figures show that visits fell sharply in March and April, at both major A&E departments (type 1) and minor A&E departments (types 2 and 3, which include urgent care centres and a small number of specialist A&E departments). The absolute fall in visits relative to the same month the year before is larger for major units (12,000 in March and 21,000 in April) than minor units (9,000 in March and 18,000 in April). But the percentage changes are larger for minor units. Visits to major A&E departments fell by 26% in March and 48% in April, while for minor units the drop was 35% in March and a staggering 71% in April. This is consistent with patients with less severe conditions seeking or being directed towards care outside acute settings or choosing to go without medical help.
Public Health England syndromic surveillance data on visits to major A&E departments shows that some of the drop is accounted for by a reduction in visits for infectious diseases, such as gastroenteritis and bronchiolitis/bronchitis. These have remained lower throughout the lockdown and are likely, at least in part, to reflect a true reduction in prevalence. There was a great deal of concern in April that those with acute conditions such as stroke and heart attack were not attending A&E. This led the government and Chief Medical Officer to stress the importance of going to hospital if you develop acute symptoms. Fortunately, the signs are that at least for these conditions, the numbers of visits have returned or are returning to their long run averages.
Emergency admissions via A&E
Moving on to emergency admissions from A&E by type, we can see that most admissions from A&E are through major units. Admissions from major units fell by 22% in March and 37% in April, although these were smaller percentage falls than the reduction in A&E visits. The emergency admission rate will be affected by the number of people who attend A&E, what conditions they have and how unwell they are, all of which have been affected by COVID-19. However, the COVID-19 pandemic may also affect decisions about who to admit, as clinicians seek to keep patients out of hospital where possible, to reduce risks of non-COVID patients being infected and to protect capacity. The drivers of these changes should become clearer when we are able to examine patterns by condition.
Ambulance incidents
In contrast to A&E visits, ambulance incidents increased by 5% in March before falling by 4% in April. This highlights that patient responses to COVID-19 are having different impacts across different services. Even though the changes in the numbers of incidents were small relative to the large shift in A&E visits and emergency admissions through A&E, there were large shifts in how the ambulance service cared for patients. In particular, there was a fall in the absolute number and the percentage of incidents that resulted in patients being transported to A&E. The number of patients transported to A&E by ambulance in April 2020 was 29% lower than in April 2019. This is a reduction of 4,000 patients per day or 120,000 across the whole month which amounts to 19% of the overall drop in A&E visits at major units in April 2020 relative to April 2019.
Ambulance crews are instead treating an increasing number of patients at the scene. The number of incidents outcome was ‘see and treat’ or ‘hear and treat’ increased by 39% in March and 37% in April relative to the same month the year before. Overall, the percentage of ambulance incidents that resulted in transport to A&E fell from 59% in both March and April 2019 to 48% in March 2020 and 44% in April 2020. This is a very rapid change to how the ambulance service provides care over a very short time period.
What can these early data tell us?
These A&E and ambulance data demonstrate the scale and speed of the changes in NHS emergency care in the first 2 months of the COVID-19 pandemic. They also show that understanding why those changes have happened is complex. How the NHS treats patients has changed, but so too has how patients seek treatment and the underlying rates of some diseases.
Over the next few months, we will use data from more services as they become available, in order to provide a more granular and complete picture of how patients and the health and social care system are adapting to these unprecedented changes.
Elaine Kelly (@ElaineKTHF) is Head of Economics Research at the Health Foundation.
Zoe Firth is an Economics Analyst at the Health Foundation.
Further reading
Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
View current vacanciesThe Q community
Q is an initiative connecting people with improvement expertise across the UK.
Find out more

