Exploring the fall in A&E visits during the pandemic
30 June 2020
Key points
- COVID-19 has led to radical changes in the way people are using NHS and social care services, and emergency care is no exception.
- At the start of the outbreak the numbers of people attending A&E fall sharply to 52% below normal. By mid-May A&E visits had increased but were still 36% lower than expected for this time of year.
- Three potential reasons behind reductions in A&E visits are: changes in how NHS services operate, changes in patient behaviour and changes in the prevalence of conditions.
- Reductions in visits predate lockdown, suggesting that initial reductions were not a reaction to lockdown itself but instead to an increasing awareness of COVID-19.
- Visits for ‘any type of injury’ fell to a low of 65% below normal, far lower than the 44% seen for visits related to ‘illness’.
- Some of the greatest reductions are for more minor injuries such as sprains/ligament injuries and muscle/tendon injuries, where visit levels fell by 81% below normal just after lockdown was announced (25 March).
- For most illness diagnoses, there were initial reductions to between 40–60% below normal from mid-March to early April and recoveries to 15–30% below normal by mid-May.
- For infectious diseases and other diagnoses related to infections, including respiratory conditions, levels of attendance remain 40–55% below normal. This is likely, at least in part, to represent a true reduction in prevalence as a result of the lockdown.
- Overall, multiple factors are driving attendance reductions. There has likely been a true reduction in the prevalence of some illness and injury types, but patient and system behaviours have also played a role.
Introduction
Over the last few months we have seen radical changes to NHS and social care services, and to our everyday lives due to the coronavirus (COVID-19) pandemic. We know that at the national level visits to major A&Es in April 2020 were 48% lower than in April 2019, with similar reductions at a regional level. We would expect social distancing measures to have a significant impact on population health, with reductions in infectious diseases and in certain types of injuries. However, we would expect the prevalence of other illnesses and injuries, such as chronic conditions, to remain constant. We might also expect both patients and health and social care workers to be concerned about infection risk in hospitals, leading to increased efforts to seek and direct patients to care elsewhere. This is important, as if more appropriate care is being given outside of A&E, this may be something the NHS should retain.
Understanding what has driven the reduction in visits helps us understand the wider health impact of COVID-19. We know that the UK is seeing increased numbers of excess deaths (deaths over and above the number expected in a given period), some of which may be attributable to reductions in A&E visits. Insights can also be used to inform future government messaging around when and how the public should seek emergency care.
What could be driving the reduction of A&E visits?
We previously outlined three potential drivers of changes that might be driving the reduction in A&E visits:
- Policy choices made in order to create capacity for COVID-19 patients or to protect non-COVID patients and staff.
- Changes in patient behaviour.
- Changes in the prevalence of some conditions.
Here, we use data of visits at 39 major (type 1) A&E departments in England to explore what is driving the reduction. These units have been chosen because they consistently include patient diagnoses for at least 75% of visits and report data in a timely manner. The data is split by type of attendance (illness/injury/nothing abnormal/not recorded) and within illness and injury by diagnosis.
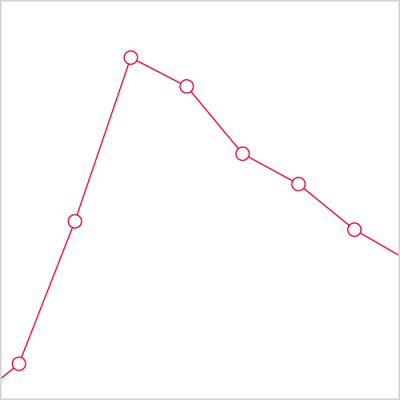
We see a significant fall in visits at these A&E departments in line with trends seen nationally. The reduction in visits starts 2 weeks prior to lockdown, falling to 52% below normal. Visits start to rise to 36% below normal by mid-May. This suggests it is reasonable to use the data as the basis for understanding patterns across England as a whole.
Types of visit
The majority of visits at A&E are categorised as being due to illness (46.3%) or injury (35.0%). Small proportions of visits are coded as ‘nothing abnormal detected’ (9.1%) or ‘diagnosis not recorded’ (9.5%).
Across categories of visits the overall pattern is strikingly similar. The scale of the initial reduction and subsequent rise in visits varies, but the timings and overall shape remain remarkably consistent. Injury visits fell to 65% below normal just after lockdown was announced, increasing to 40% below normal by mid-May. Illness visits fell to 44% below normal but the reduction took longer, reaching the lowest point in mid-April. By mid-May illness visits had increased to 31% below normal.
It is also notable that for the vast majority of diagnoses the reduction starts 2 weeks prior to lockdown. This suggests that the initial reductions are not a reaction to lockdown itself, but a response to increased awareness of COVID-19 in society and the health care and social care system as we entered the outbreak.
As we break down illness and injury visits by diagnosis, we start to see greater variation.
Injury
Within injury visits we see an initial reduction in visits followed by a rise across all diagnoses. However, it is possible to identify two groups of diagnoses that follow similar patterns.
Firstly, there is a group of injury diagnoses that likely include a significant number of sporting or playground injuries: contusions, fractures, muscles/tendon injuries, soft tissue inflammation and sprain/ligaments. For these, we see an extreme initial reduction to 60–81% below normal. Visits across all diagnoses then start to recover but by mid May are still significantly below normal (52–41%). Soft tissue inflammation is a slight outlier, falling to 63% below normal initially but with a greater recovery to 26% below normal. This is consistent with children no longer attending school or extra-curricular activities, and adults taking part in fewer sports. There also seems to be a link to severity of injury: for example, muscle, tendon, sprain and ligament injuries see slightly greater reductions in comparison to fractures. The large reduction in more minor injuries is also consistent with patterns in national data that show larger reductions in visits to minor A&E departments, which often treat these injuries.
By contrast, other injury diagnoses see a smaller reduction initially (44–54%) and a recovery to near normal (8–29%) by mid May. These include ophthalmology and faciomaxillary, common household or workplace injuries (burns, scalds and lacerations), and foreign body and poisoning.
Illness
With three notable exceptions (see below), all illness diagnoses follow the pattern described above: an initial reduction followed by a recovery in attendance numbers. We see significant variation in the scale of the reduction and recovery, with few obvious groupings.
That said, for the vast majority of illness diagnoses, we see initial reductions of between 40–60% below normal and recoveries to 15–30% below normal. If we take cardiac conditions as an example, visits fell to half their normal rate and have recovered to ~75% of normal. The decrease in cardiac visits has been noted with some concern by cardiologists, 85% of whom believe the drop in heart attack visits is due to fear of catching COVID-19. Public Health England data seems to show a corresponding rise in ambulance calls relating to cardiac/respiratory arrest, and to a lesser extent chest pain.
This may be consistent with those with less severe symptoms calling 999 prior to an A&E attendance, to see if they can seek care outside acute settings. The reduction in A&E visits could then be due to only those with the most severe symptoms attending A&E. Without further research it is difficult to know for sure.
COVID-19
As expected, for COVID-19 visits we see a dramatic rise in visits that begins the week prior to lockdown and coincides with the reductions in other areas. The peak in visits is reached 2 weeks into lockdown and falls from there. Even at their peak, COVID-19 visits accounted for only 9.9% of illness visits and 2.7% of overall A&E visits.
Infectious diseases and respiratory conditions
For infectious diseases (non-COVID 19) and respiratory conditions, we see a different pattern. Here, there is a slight percentage increase in visits 2 weeks before lockdown, the time visits for other illness and injury diagnoses are starting to decrease. This could indicate a rise due to undiagnosed COVID-19, but it is difficult to draw firm conclusions. We then saw a reduction to ~50% of normal that has remained constant into mid-May. There is no indication that visits for these conditions are returning to normal, as seen in other illness and injury diagnoses.
We see similar trends in Public Health England surveillance data, with reductions in A&E visits for respiratory infections, bronchiolitis, flu-like symptoms, pneumonia and asthma, and in the prevalence of the majority of notifiable infectious diseases. We are also able to get a sense of whether people are seeking treatment elsewhere for some of these conditions. We see no increase in GP visits for respiratory conditions, indeed visits are down for respiratory infections, pneumonia and asthma – patients do not seem to be going elsewhere. This is also the case for gastroenteritis and infectious diseases such as chickenpox.
Reductions across these areas do not predate lockdown, instead seeming to be a reaction to it. Indeed, we would expect social distancing to reduce the prevalence of these diagnoses. Although social distancing was introduced to slow the rate of transmission of COVID-19, it has slowed the rate of transmission of other communicable diseases. It is, therefore, reasonable to assume that there has been a true reduction in prevalence of other infectious diseases.
A complex overall picture
Rightly, there has been considerable concern about the drop in A&E visits. However, reviewing data by the type of attendance and diagnosis indicates a complex overall picture, and one that is linked to the three potential drivers: changes in how NHS services operate, changes in patient behaviour and changes in the prevalence of conditions.
Firstly, we know that there have been changes to how A&E departments operate. A March 2020 NHS England briefing recommended separate pathways for patients who present with respiratory symptoms and those without, reducing emergency admissions for non-respiratory patients where possible. While there is no suggestion that A&Es should take any steps to reduce the number of patients who attend, there are indications that patients may have been able to seek appropriate care elsewhere. We know, for example, that an increased number of 999 calls are resulting in treatment at the scene, and that fewer NHS 111 calls are resulting in a referral to A&E. This may reflect an increased desire both on the part of patients and heath care professionals to treat outside of hospital. It may be possible to retain these changes in future, helping to reduce pressure on A&E departments over the long term, although further research is needed to understand the impact on patient outcomes.
Secondly, there is emerging evidence of changes in patient behaviour. Research by Ipsos MORI for the Health Foundation, between 1 and 10 May, found that 47% of the public would feel uncomfortable using their local hospital if the need arose – three-quarters of whom due to concern about exposure to COVID-19. A key question though is whether those who chose not to attend A&E should have done.
Unfortunately, it seems likely that in at least some cases non-attendance at A&E has caused patient harm and is undesirable, such as in the case of cardiac conditions. This may have led to some of the excess deaths we have seen, although at this stage we cannot be sure. However, in other cases patients may have been able to seek more appropriate care elsewhere. The more sustained reductions in visits for minor injuries such as sprains and muscle/tendon injuries, and greater attendance reductions at minor A&Es (types 2 and 3), may indicate this has taken place. Further research is needed to understand the extent of patient harm caused by non-attendance at A&E.
Finally, our data does indicate that in some instances there has been a true reduction in the prevalence of conditions that would normally lead to an A&E visit. Respiratory conditions and infectious diseases are notable examples of this. In these instances, we would not expect a non-attendance to have caused worse outcomes. It also means that there will likely be little or no ‘pent-up’ demand from these conditions. However, it also means that these reductions are unlikely to remain once lockdown is lifted and the NHS will need to be prepared to manage an increase in these types of visits as restrictions are lifted.
It is also worth noting that COVID-19 visits, even at their peak, accounted for only a very small proportion of overall visits. A&Es were not overrun by COVID-19 patients, and this is an important message for A&Es and the wider public, concerned about capacity.
Looking ahead
COVID-19 will have a lasting impact across society, and emergency care is no exception. In the short term, the need for social distancing will mean that A&Es will not be able to operate as previously. We may well also see an increase in demand in some areas due to cancellations or delays from other parts of the health care system (for example the large number of delayed elective procedures, although our data does not seem to indicate that this pent-up demand will come from non-attendances at A&E).
Insights from attendance data should now be used to inform plans for how A&Es will adapt to post-lockdown operation, including for a potential second wave of COVID-19 infections. Over the longer term, we must consider whether a return to ‘normal’ is desirable. COVID-19 may provide us with a chance to achieve a sustained reduction in non-urgent A&E visits, something that has been unachievable previously. Overall, it is important that we continue to monitor and understand changes in visits. This will ensure any decisions about the future of emergency care are made using the best possible evidence.
Ruth McConkey is a Programme Manager for the Economics team at the Health Foundation.
Steven Wyatt is Head of Strategic Analytics at The Strategy Unit.
Further reading
Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
View current vacanciesThe Q community
Q is an initiative connecting people with improvement expertise across the UK.
Find out more

