Public perceptions of the NHS and social care: performance, policy and expectations
Public perceptions of the NHS and social care: performance, policy and expectations
3 February 2022
Key points
- The COVID-19 pandemic has caused major shifts in public attitudes towards health, the NHS and social care. With services still experiencing substantial pressure from the virus itself and related disruption, it’s important to understand how people perceive the current state of care and priorities for the future.
- This long read examines public perceptions and expectations of health and social care. It highlights key findings from the first wave of our new programme of polling research, delivered in partnership with Ipsos, that will track public views on health and social care every 6 months.
- Our first public poll was conducted between 25 November and 1 December 2021, with a total of 2,102 responses from people aged 16 and older across the UK via Ipsos’ KnowledgePanel, a random probability online panel.
- The public is pessimistic about the state of the NHS and social care. 57% think the general standard of care provided by the NHS has got worse in the last 12 months, while 69% think the standard of social care services has deteriorated. Expectations for the next 12 months are slightly less pessimistic but still low: 43% think NHS standards will get worse, while 53% think the same about social care.
- In previous years local NHS services have been viewed more positively than the NHS overall, but this is no longer true: perceptions of the service locally and nationally are now very similar. Less than half think the NHS is providing a good service nationally (44%) or locally (42%).
- While the government is yet to commit to a plan for addressing long-term NHS staff shortages, expanding and supporting the workforce is a pressing issue for the public. People’s top priorities for the NHS include addressing the workload pressures on NHS staff, increasing the number of staff in the NHS and improving waits for routine services.
- In England, the government has put protecting the NHS at the centre of the pandemic response, begun a wide-ranging reform agenda and committed substantial additional funding. However, few people (9% in England) think the UK government has the right policies for the NHS.
- Although at the time of the fieldwork the policy was yet to come into effect, 58% of the public support the government’s decision to raise taxes to spend more on the NHS and social care, with only 22% opposing it.
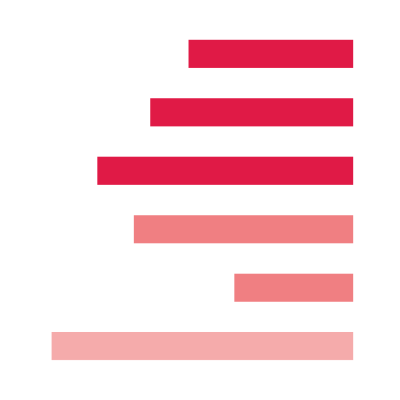
Figure 1
Standards of care over the next 12 months
Looking ahead, the public is more optimistic about whether the NHS will improve – albeit only slightly. Nearly one in five (18%) expect the general standard of NHS care to get better in the next 12 months, while 43% expect it to get worse. This is considerably worse than in May 2020, when only 25% expected the standard of care to get worse – however, that coincided with the peak of the first wave of COVID-19, when people were clapping for carers, so may have reflected a surge of optimism. The latest results are closer to expectations in May 2017 and November 2019, when 48% and 37% of the public respectively expected the standard of NHS care to get worse. In this respect, expectations could be said to have returned to normal – at least, prior to the latest wave of the pandemic.
When considering different aspects of the NHS, the public is most likely to think the pressure on NHS staff (67%), waiting times for routine services (63%), the wellbeing of NHS staff (60%) and waiting times for A&E (59%) will get worse over the next 12 months. People are least negative about the prospects for the standard of care at their GP practices (42%) and local hospitals (38%) – but only 12% and 11% respectively think standards will improve. And, as above, those living in the most deprived areas are more likely to think standards of care at their GP practices (53%) and at hospitals (46%) will get worse.
People are more pessimistic about the prospects for social care than for the NHS, with 53% expecting the general standard of care to get worse over the next 12 months. This is considerably more than in May 2020 (31%), but may be a further sign of expectations returning to levels typically observed before the pandemic – 50% in May 2017 and 40% in November 2019. While both surveys were conducted in the context of general elections, social care as a campaign topic played out very differently in England – Theresa May’s proposals for reform sparked controversy in 2017, whereas Boris Johnson’s promise to ‘fix social care’ (without specifying how) effectively neutralised the issue in 2019.
Further reading
Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
View current vacanciesThe Q community
Q is an initiative connecting people with improvement expertise across the UK.
Find out more

