What has been the impact of COVID-19 on care homes and the social care workforce? COVID-19 chart series
15 May 2020
- Office for National Statistics (ONS) data released this week highlight significant weaknesses in the social care system. High death rates sustained during the COVID-19 pandemic demonstrate the stark impact of the virus on care home residents and social care workers.
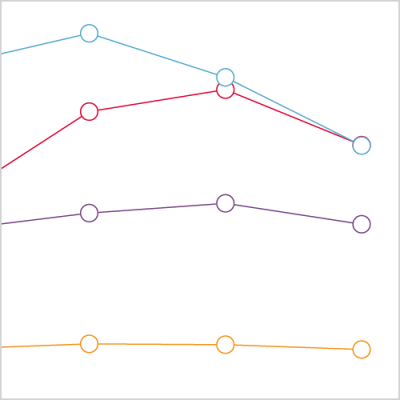
- While deaths in hospitals have declined from a peak in the week ending 17 April, COVID-19 has continued to spread in care homes. In the week ending 1 May, the number of deaths in care homes from all causes (6,409) exceeded the number of deaths in hospital (6,397) for the first time since the start of the outbreak.
- The outbreak is also having a devastating impact on people working in social care. When adjusted for age and sex, social care workers have twice the rate of death due to COVID-19 compared to the general population.
- Between 10 April and 8 May, 3,161 people receiving domiciliary care in the community died. This is over twice the number expected (1,171 deaths) at this time of year.
- Action to tackle the coronavirus pandemic in social care has been late and inadequate. The government has announced a package of £600m available for infection control in care homes. It is vital that this reaches front line providers and that the huge practical challenges of personal and protective equipment (PPE) and testing logistics are resolved.
- Care homes includes homes for the chronic sick; nursing homes; homes for people with mental health problems and non-NHS multi function sites.
- Deaths at home are those at the usual residence of the deceased (according to the informant)‚ where this is not a communal establishment.
- Hospices include Sue Ryder Homes; Marie Curie Centres; oncology centres; voluntary hospice units; and palliative care centres.
- Hospital includes acute or community, not psychiatric.
- Other communal establishments include schools for people with learning disabilities; holiday homes and hotels; common lodging houses; aged persons’ accommodation; assessment centres; schools; convents and monasteries; nurses’ homes; university and college halls of residence; young offender institutions; secure training centres; detention centres; prisons and remand homes.
- Elsewhere includes all places not covered above such as deaths on a motorway; at the beach; climbing a mountain; walking down the street; at the cinema; at a football match; while out shopping; or in someone else's home. This category also includes people who are pronounced dead on arrival at hospital.
Source: Office for National Statistics, Deaths registered weekly in England and Wales, provisional.
What does the latest data tell us about deaths in care home?
Deaths in hospitals have declined from a peak of 9,434 in the week ending 17 April, to 6,397 in the week ending 1 May. However, the outbreak has continued to spread in care homes. As the above chart shows, there were 6,409 deaths in care homes in the week ending 1 May, exceeding the number of deaths in hospitals (6,397) for the first time since the start of the outbreak.
However, this is likely to be an underestimate of the scale of the impact of COVID-19 on care home residents. Data published on 15 May show that a total of 45,899 care home residents have died since the start of the pandemic, 12,526 from COVID-19. This includes 3,444 care home residents dying in hospital. The large increase in the number of deaths from all causes since the outbreak began is likely to be a more accurate indication of the scale of the direct and indirect impacts of the pandemic on those living in care homes.
What’s the impact on the social care workforce?
When adjusted for age and sex, social care workers are more than twice as likely to die from COVID-19 compared to the general population. In contrast, staff working in the health care sector do not appear to have a statistically significant raised risk of death compared to the general population.
However, there are some important limitations that need to be explored further. Some deaths may not have been registered as they are still under review by the coroner. Our analysis only includes deaths registered up until 20 April, so death rates for both social and health care workers are likely to change considering the sustained high number of deaths. Workers aged 65 and over were also excluded from the analysis. While any of these factors alone are unlikely to explain the total raised mortality rate seen in social care workers, they may change the relative difference seen between health care and social care workers.
Caution is also required when comparing death rates for social and health care workers without considering that averages may hide significant differences between different types of workers within each industry. And for all staff, there are likely to be significant other adverse impacts, including from burnout and mental health issues.
Why might those receiving and working in social care be more at risk?
The high death rates sustained over the pandemic demonstrate the stark impact of COVID-19 on care home residents and social care workers.
Infection control and isolation in care homes and private homes is much more difficult than in the controlled, clinical environment of a hospital. People receiving social care often have underlying conditions that make them more at risk of infection and death from COVID-19. Some people require physical help with aspects of daily living such as washing or eating, making complete isolation very difficult.
Social care workers are often poorly paid and on insecure contracts. The sector is also hugely fragmented with thousands of organisations providing care, with concerns being raised about adequate provision of personal and protective equipment (PPE) for staff in care homes. Social care workers often need to have very close physical contact with those they care for, and in care homes many people live in the same building or facility. This makes transmission of the virus among staff and patients more likely.
What is needed?
Weekly deaths from COVID-19 in care homes are starting to decline slowly, but the virus is still circulating in hospitals, care homes and the community. To prevent a resurgence in cases, there is a clear need to better understand the causes of transmission in both care home workers and residents.
Since 29 April, deaths in care homes are being reported daily, but there is still a lack of information on the numbers of cases and tests in care homes. Outside of care homes, we now know that between 10 April and 8 May 2020, there were 3,161 deaths of recipients of domiciliary care in England. This is over twice as high as the three-year average (1,171 deaths) for the same period. However, there is no published and timely information on COVID-19 cases, hospital admissions or deaths for this group of people. Additionally, we don’t fully understand the impact on those receiving social care in the community, or people with unmet need for care, including those with learning disabilities.
The government has announced a package of £600m available for infection control in care homes. This is welcome as there have also been reports of a lack of PPE for staff, along with testing issues in care homes, which has restricted the effectiveness of the response. It is vital that they make sure this reaches front line providers and that the huge practical challenges of PPE and testing logistics are resolved.
Further reading
Learn more
Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
View current vacanciesThe Q community
Q is an initiative connecting people with improvement expertise across the UK.
Find out more

