Do all care home residents face an equal risk of dying from COVID-19?
22 May 2020
Key points
- The coronavirus (COVID-19) pandemic has disproportionately affected care homes in different regions across England.
- The highest number of deaths among care home residents occurred in the south-east of England. However, once the number of care home beds in each region are taken into account, it appears that care homes in northern England and London have had more deaths relative to the number of care home beds than other areas.
- In the north of England a higher proportion of care homes are found in more deprived areas, which might be reflected in increased vulnerability to COVID-19 among care home residents and staff.
- More granular and up-to-date data are needed to fully understand the impact of COVID-19 on care home residents and staff across different regions, and to inform decisions on how to allocate resources where they are most needed.
- Data systems fragmentation, lack of data flows and systematic under investment in data and technology must be urgently addressed by government if a resilient and fit-for-purpose social care system is to be built.
Care homes have been on the front line of the COVID-19 outbreak. Those living and working in care homes are more vulnerable to the virus than the general population. Residents are often frail with underlying health conditions, and infection control and social distancing is more difficult in what is someone's home, not a hospital.
The sector is also fragmented with thousands of organisations providing care, the social care sector as a whole having suffered from years of historic underfunding, and with a workforce often on low pay and insecure contracts. These factors should have motivated urgent support by the government to ensure that care homes had the PPE, testing and advice they needed. But by April it was becoming increasingly clear that action came too late to stem the tide of deaths.
Figures from the ONS have since shown that by 1 May there were 12,526 COVID-19-related deaths among care home residents in England and Wales. While recent data indicate that the situation in care homes may be stabilising, all-cause mortality remains dramatically above the 5-year average. And without a vaccine, the virus may be with us for some time, so despite the falling number of deaths there is no room for complacency.
To date the focus has been on the national picture. But this may hide significant variation between care homes and regions. In this analysis we examine which areas of the country have been hit hardest and suggest possible reasons behind these differences.
Where have the greatest number of care home deaths occurred?
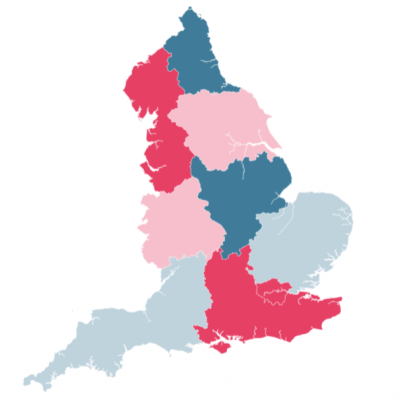
More COVID-19-related deaths among care home residents occurred in the south-east of England than any other region, with fewest in the north-east, as shown in Figure 1. To date, 2,109 deaths among care home residents in the south-east were identified as COVID-19 related, representing 18% of the total COVID-19 death toll among care home residents in England. Without taking into account the size of the care home population, this is more than twice the number of deaths in the north-east, which had 827 COVID-19 deaths among care home residents (7% of the national total).
The proportion of care homes that have reported COVID-19 outbreaks in the south-east of England is 37%, which is close to the national average of 38%. The percentage of care homes affected varies widely between regions, from 27% in the south-west to almost double (49%) that in the north-east. This suggests that while the total burden from the epidemic in terms of loss of life may have been greatest in the south-east, the total spread and local impact of COVID-19 in the north-east may be greater than it appears.
Care homes in London, the north-east and north-west of England have been more affected by COVID-19
A relatively simple explanation for this apparent difference in the total number of deaths might be the size of the care home population in each region. In England, there were a total of 15,494 CQC-regulated care homes in April 2020, with a capacity of 456,862 beds. However, much like the general population in England, care home beds are not equally distributed across the country. While around 19% of care homes are in the south-east, only about 6% are in the north-east.
We used the number of care home beds in each region to estimate the number of people living in care homes in each region. After adjusting for this a different picture emerges, with London and the north-east having the greatest number of deaths per care home bed and the south-west having the least.
Table 1: London and the north-east had the greatest number of COVID-related deaths per care home bed
| Region | Care home beds | COVID 19-related deaths (care home residents only) | Deaths per 100 care home beds | COVID-19 deaths (all) |
|---|---|---|---|---|
| London | 35,340 | 1,654 | 4.68 | 7,405 |
| North-east | 26,191 | 827 | 3.16 | 1,919 |
| North-west | 62,129 | 1,899 | 3.06 | 5,464 |
| West Midlands | 48,619 | 1,372 | 2.82 | 4,263 |
| Yorkshire and the Humber | 47,470 | 1,184 | 2.49 | 3,089 |
| South-east | 85,503 | 2,109 | 2.47 | 5,086 |
| East of England | 51,841 | 1,066 | 2.06 | 3,515 |
| East Midlands | 43,426 | 881 | 2.03 | 2,528 |
| South-west | 54,584 | 997 | 1.83 | 2,185 |
Source: CQC, care home registrations; ONS, Deaths within the care sector involving COVID-19, England and Wales, 15 May 2020; ONS, Deaths registered weekly in England and Wales, provisional: week ending 8 May 2020.
If the impact of COVID-19 on care home residents were equally distributed across the country, we would expect the number of deaths to be proportionate to the number of beds or the size of the care home population. This is not reflected in the latest mortality figures and, compared to the predicted number of deaths based on bed capacity, some areas of the country seemed to be hit disproportionately hard. Among these, London, the north-east and the north-west have had a higher number of COVID-19-related deaths than predicted using this relatively crude method, and the south-east, east Midlands and east of England have had fewer.
Although these estimates clearly point towards regional variation in the impact of COVID-19 on care homes, they need to be interpreted with caution. Total bed capacity is likely to be an overestimate of the care home population, as not all care home beds might be occupied, and accurate estimates on the number of COVID 19-related deaths relies on correct attribution on death certificates. As outbreaks are also likely to cluster within care homes, by assuming they are equally spread across care homes in the same area, there is a risk of underestimating the impact of COVID-19 on individual care homes.
Some variation in the impact of COVID-19 will reflect how the outbreak spread through different parts of the country and how early and efficiently care homes were able to reduce likely routes of transmission from the community and from hospitals. There was large variability in the total number of COVID-19 deaths across different regions (Table 1), with the most seen in London. Similarly, the proportion of COVID-19 deaths among care home residents, which was 36% nationally, varied from 22% in London to 46% in the south-west. This might reflect local variation in transmission routes in the population, population density in the community, the stage of the spread of the virus at the start of the lockdown, and the relative importance of different care settings in the spread of COVID-19.
Along with the geographical location of the care home, other factors relating to care home staff are also likely to play a role, including their own health and vulnerability to COVID-19, their living conditions and their likelihood of having second jobs inside or outside of social care.
The health needs, age, frailty and underlying health conditions of care home residents could also vary across the country. Some parts of the country could have a higher proportion of care home residents with dementia or underlying heart conditions, for example, which could place them at higher risk of severe infection. This could account for some of the variation as some underlying conditions appear to increase the risk of mortality from the virus.
However, beyond the individuals living and working in care homes, the resilience of the local sector – and the ability of individual providers to adapt and limit the spread of COVID-19 – may depend on financial and organisational resources, such as their ability to procure PPE. It may also depend on variation in access to testing for staff and residents in a region. We do not yet have detailed information on staffing, testing, PPE provision, or policies of individual care homes to fully understand these differences, but this should be an area of focus for data collection and future analysis.
More care homes are in deprived areas in the north-east and north-west of England
Socioeconomic deprivation could be linked to many of the factors listed above, such as underlying health conditions of staff and residents, or the resilience of the local sector. The English Index of Multiple Deprivation reflects some geographical inequalities closely linked to vulnerability to COVID-19, such as health and housing. Across the whole population in England, COVID-19 mortality rates in the most deprived 10% (55 per 100,000 of population) are already more than twice as high as those in the least deprived 10% (26 per 100,000 of population). Regional differences in deprivation among care home staff and residents might therefore be one of the factors underlying the variation in the impact of COVID-19.
At a national level, the locations of care homes are relatively evenly distributed across deprivation quintiles, but the proportions vary widely between regions. Compared to the south of England, more care homes in the north of England are in underprivileged areas, which might reflect an increased vulnerability to COVID-19 among care home residents and staff.
Protecting care homes across all regions
To better understand the effect of COVID-19 on care home residents, just as on the general population, it is crucial to go beyond the national picture, recognising that certain groups and geographies are more at risk in terms of exposure to infection and outcomes. The toll of COVID-19 has not been evenly spread across the country. Care home residents in the north-east and London have been particularly badly hit.
The government has announced an action plan for social care, and a further £600m in support. It is vital that this money goes where it is needed, and that ongoing problems reported by care homes in securing testing and PPE are urgently resolved. Our analysis also shows that some areas of the country may be in more need of support than others.
It is not possible to understand the scope of the issue in care homes, including which care homes are most vulnerable and why, without more granular and up-to-date data on care homes, their residents and staff. Mirroring the underinvestment in the social care workforce, there has been systematic underinvestment in data and technology in social care. Data systems are fragmented, without data flows that support decision making. Consequently, local and national leaders struggle to understand why some areas are harder hit, and act quickly to support residents and staff.
But short-term action in response to the pandemic is no substitute for building a resilient and fit for purpose social care system for the future – with a well-paid and valued workforce, supported by data and technology. The government need to make sure that social care is a service that all those in need can rely on, whoever they are and wherever they live in the country.
With thanks to Karen Hodgson and Joshua Kraindler for their helpful comments at review stage.
Fiona Grimm (@fiona_grimm) is a Senior Data Analyst at the Health Foundation.
Sarah Deeny (@SarahDeeny) is Assistant Director of Data Analytics at the Health Foundation.
Further reading
Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
View current vacanciesThe Q community
Q is an initiative connecting people with improvement expertise across the UK.
Find out more

