Turning the supertanker Finding the sweet spot for NHS quality and cost
17 July 2014

The NHS is often compared to a supertanker – huge and slow moving – but, in at least one regard, this analogy doesn’t work. That area is money. Whilst the sums involved in health care are huge, the financial position has a horrible habit of deteriorating very quickly.
Later this month the Department of Health will publish the audited accounts for 2013/14. They are likely to show a small balance but with increasing pressures below the surface. With 40% of acute hospitals in deficit, surpluses across providers and commissioners falling, savings plans underperforming, ongoing deficits and a growing reliance on one-off savings – the dark clouds are looming.
And the NHS England board papers for 3 July report that clinical commissioning groups and NHS England’s own direct commissioning spend are currently projecting a combined overspend of £137m against their total £97.3bn spending limit for the year.
Even if NHS finances limp through the current year, the numbers in 2015/16 just don’t add up. This is not a case of a few providers and commissioners having weak financial management. There is a systemic problem as the gap between the ambitions for the NHS and the resources available grows ever wider.
Recent reports in the media indicate a gap of up to £2bn in 2015/16. This is based on the numbers in the NHS planning guidance.
Key figures for the NHS' circa £80bn secondary care budget
| 2014/15 | 2015/16 | 2016/17 | 2017/18 | |
|---|---|---|---|---|
| Total affordability challenge | 3.1% | 6.6% | 5.5% | 4.7% |
| Provider efficiency | 2.0% | 2.5% | 2.0% | 2.0% |
| System efficiency | 1.0% | 2.0% | 1.0% | 1.0% |
| Remaining challenge | 0.1% | 2.1% | 2.5% | 1.7% |
If NHS providers manage to deliver a very respectable further 2.5% efficiency improvement in 2015/16 and there is a further system efficiency of 2% (which is above recent experience and expectations for every other year), there is a gap of £1.6bn. If system efficiency is at the more probable 1%, the gap is over £2bn.
An injection of £2bn in 2015/16 would get the NHS back to an efficiency requirement of around 4% – almost double the Office for Budget Responsibility’s assessment of the trend rate of productivity growth for the UK economy as a whole (2.2% as per the OBR’s Fiscal Sustainability Report in July 2014). It’s a lot of money to get the NHS back to a really tough financial position. But it’s also a big ask for overall government spending.
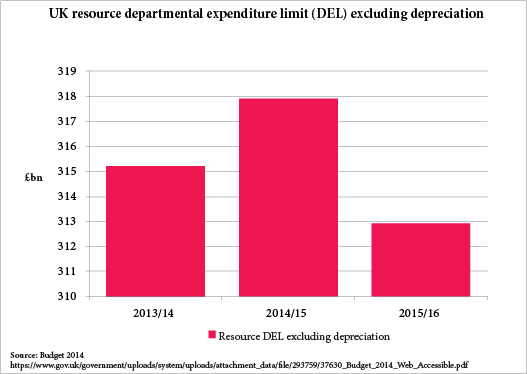
The chart below shows the government’s plan for current spending on all public services up to 2015/16, as announced in the Chancellor’s budget statement in March this year. All the pain from cuts to public services will result in a reduction in spending of £5bn in 2015/16. To then inject £2bn in to the NHS would undo much of that fiscal consolidation.
Whatever happens to the precise funding of the NHS in 2015/16, the stark fact remains that the NHS faces a very large efficiency challenge. It is also clear that the pressure to improve quality is not going away. Over the last year quality and financial balance have often been presented as alternative priorities for the NHS. Of course, in many cases, improved quality requires more resources and so measures to reduce cost can have a negative impact on quality. But the relationship between cost and quality is more nuanced than stark alternatives.
At the Health Foundation, we commissioned Professor John Øvretveit to review the evidence on the cost and quality relationship: Does improving quality save money?, Does clinical coordination improve quality and save money? and Do changes to patient–provider relationships improve quality and save money?.
The studies reported a few years ago but the key messages are very relevant to today’s challenge. The research shows that despite a dearth of robust costing evidence there are some examples of interventions that showed increased (and maintained) quality whilst reporting savings, even after taking into account the cost of the intervention.
The most promising interventions included reducing clinical variation, redesigning clinical roles/multidisciplinary and collaborative approaches to tacking specific quality problems, and targeted measures to reduce waste/running costs, such as efforts aimed at reducing delays and cancellations, as well as improved discharge regimes. The strongest evidence generally comes from studies that seem to align most closely with Monitor’s ‘improving productivity within existing services’ categorisation of closing the funding gap opportunities. Importantly, many of the interventions in these exemplar studies were set within organisations that had an overarching and strong culture of quality improvement. The research is also a reminder that harm is expensive. So reducing adverse drug events, tackling pressure ulcers and falls, better communication and management of patients at discharge all have benefits for efficiency and quality.
Whilst portals like NHS Evidence make it easier to link practitioners to research, it is very difficult to find much new, systematic evidence from the last few years on effective interventions to simultaneously improve quality and efficiency, despite this being fundamental to the sustainability of the NHS.
Realising savings and improving quality also depend on effective implementation, and national leadership on this issue has been limited. The Health Foundation has been doing what it can and the Shine programme provides some very encouraging examples of local initiative. But charities, commissioners and providers should not have to do this on their own. Alongside their initiative we need a national, systematic effort to improve the evidence on the quality/cost ‘sweet spot’.
As NHS commissioners and providers develop their plans for 2015/16, surely whatever else we do across the NHS we need to relentlessly focus on this quality improving/cost reducing sweet spot. It won’t solve the funding gap but it is part of ‘thinking like a patient and acting like a taxpayer’, to quote Simon Stevens.
Anita Charlesworth is Director of Research and Economics at the Health Foundation.
Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
View current vacanciesThe Q community
Q is an initiative connecting people with improvement expertise across the UK.
Find out more